When you set boundaries with clients, you protect the nurse-client relationship, your privacy, and your well-being. In the mental health setting, clients may push boundaries in different ways, typically because of the way their illness is presenting. Because you work with personalities and behavior in this field, setting and maintaining boundaries can be difficult. It requires consistency and firm communication.
There are many ways that your boundaries as a care provider can be violated:
- Verbal, physical, or sexual harassment or abuse
- Flirtatious behavior – e.g. complimenting your appearance, telling you they’ll miss you, asking for physical examinations when it is not indicated
- Asking personal questions – e.g. about your family/partner, what you did over the weekend, etc.
- Asking intrusive questions about your professional role – this can be anything outside of your credentials and whether you are qualified to perform a certain skill; e.g. your work schedule, what school you attended, etc.
- Overly friendly behavior – asking for your phone number, gift giving, constantly making small talk that does not have any therapeutic benefit
- Dependent behavior – e.g. constantly seeking reassurance for the same thing, asking to be monitored for every small task, etc.
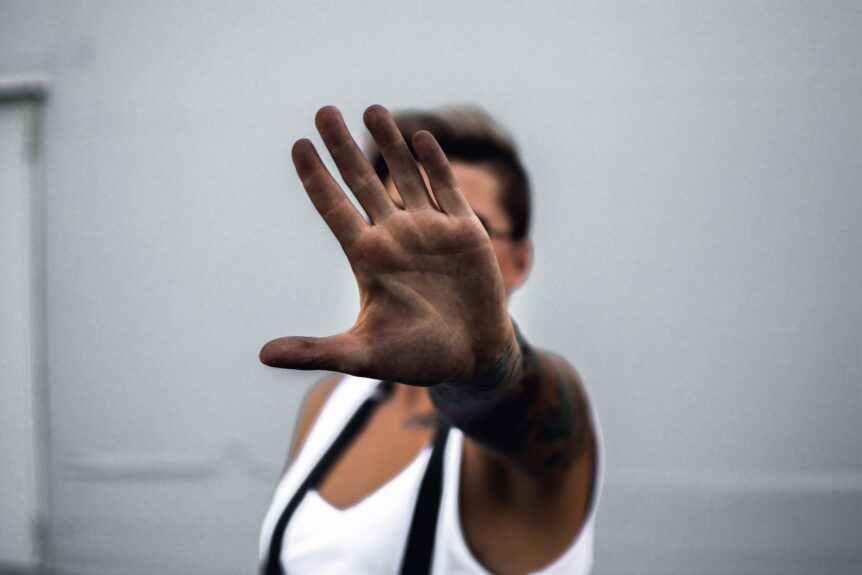
Here are 10 different ways that you can set boundaries with patients.
READ ALSO: Debunking 5 Popular Myths About Mental Health Nursing
1. Say no.
I remember feeling like I was being rude to my clients when I was too firm saying no. But being comfortable with saying this word is so important. There are other equally effective ways to get the message across: “that’s inappropriate”, “you’re not allowed to use those words”, and “that behavior is unacceptable here”. Address boundary-crossing when it first happens, and be consistent in re-addressing it so that your messaging is clear. Inconsistency can cause confusion, leading to more undesirable behavior and even aggression or anxiety.
2. Limit interactions and requests to specific frequencies.
Clients who approach you at the nursing station every 10 minutes with a new request will mentally drain you quickly. My best approach with these clients is to set a time frame for when they can approach you, for example at the top of each hour. Creating this boundary will prevent the client from growing dependent on you and other staff and help them learn how to prioritize their needs and deal with some of their needs independently too.
3. Reinforce unit or facility policies.
Rules are rules, and clients and nurses alike have to abide by them. Using indoor voices, lounge or common space restrictions, infection control procedures, and an environment of mutual respect are all examples of what can be brought up if relevant. For example, a client can’t yell at you from the other end of the hallway when they need something. They can approach you in the hallway or at the nursing station and would also need to demonstrate patience if you cannot attend to their needs immediately. Don’t tolerate inappropriate because it reinforces the behavior and will burn you out.
4. Explain why a client’s words or actions are inappropriate.
Clients are humans too, and nobody’s perfect. Sometimes your client may need a reminder or explanation about why they can’t speak or behave in a certain way. Remind them that there’s a level of professionalism expected between a nurse and a client. For example, if a client insists on exchanging phone numbers when they’re discharged, reinforce that you have to say no because of ethical and professional reasons. Explain that even when the nurse-client relationship ends, your and your client’s safety and privacy still must be maintained.
5. Address underlying issues.
Is the client anxious about being in the hospital, leading to overly-dependent behavior? Has the client been off their medications for a while before admission, leading to outbursts toward staff? Not all underlying issues can be addressed within a shift or even at all, but having an idea of the root cause can help you tailor your interventions. Taking the time to understand this can also prevent stigmatizing clients as “attention-seeking” or “difficult”.
6. Reorient the client to their surroundings.
Especially with older adults, disorientation can lead to unpredictable behavior. The client may not know where they are or who you are. Aside from verbal reminders, find strategies to help clients self-reorient to set boundaries throughout the shift. For example, if a client has a whiteboard in their room, write this on it: “Hello! You’re in ABC Unit of XYZ Hospital. Your nurse today is Crystal.” Little things like this can make a difference!
7. Have a conversation with the client.
Bring up the things that you are concerned with. Use statements like “I noticed that…” or “My colleagues and I are concerned that…” Allow the client to verbalize their side of the situation. Come to a compromise of what is realistic for their care and establish a plan moving forward. By doing this, you show empathy and involve the client in decision-making.
8. Offer one of two choices.
This method works well when a client approaches you with too many requests are unable to make concrete decisions about what they need. By offering them two choices to pick from, you help them come to those decisions faster while providing them control. At the same time, it reasserts the fact that it is not realistic for you as a nurse or care provider to bring a client 10 different snacks one after another–they’ll have to choose which one they want and respect that you have other tasks to deal with!
9. Using “first, and then” statements.
Tying into the previous tip, there are clients who require more structure when it comes to getting tasks done. Especially when someone is experienced disorganized thinking, this method can save you time and help the client move on with their goals in the day. It also helps in cases where clients are avoiding care for no apparent reason and need motivation. For example: “First I’ll give you your medication, then we can do your laundry”.
10. Disengage from the interaction.
If all other methods fail, the best thing to do is to disengage from the client. Firmly tell the client, “You’re crossing boundaries. I’ve given you a chance to stop but you didn’t, so I’m going to walk away now.” Then walk away! If the client continues to behave inappropriately in the future, limit your interactions with them and disengage again whenever the behavior returns. A little distance might be what you need to be able to set boundaries again.